Sleep apnea, a type of sleep-disordered breathing, affects millions of people worldwide. While it’s prevalent in both men and women, there are distinct differences in its occurrence, symptoms, and treatment across genders. Recognizing these disparities is essential for sleep medicine professionals and those seeking to understand their symptoms. Learn more about why.
Key takeaways:
- Diagnostic Variability: Men are frequently diagnosed with sleep apnea, but distinct symptoms in women suggest underdiagnosis.
- Physiological Differences: Gender-specific anatomical and hormonal variations influence sleep apnea risk.
- Personalized Treatment: CPAP is primary, but gender-focused strategies optimize care.
What is Sleep Apnea?

Sleep apnea refers to instances where breathing stops and starts repeatedly during sleep. The most common form is obstructive sleep apnoea (OSA), which happens when throat muscles relax excessively, causing a blockage in the upper airway.
Another term you might come across is sleep apnea syndrome, which encompasses the broader symptoms and complications of the condition.
Prevalence and Presentation in Both Genders
In the study of sleep disorders, there’s a notable trend where men are diagnosed with sleep apnea more often than women.
However, as our understanding deepens, recent data suggests that women might be underrepresented in sleep apnea diagnosis figures.
This differential can be attributed to distinct symptom presentations in each gender. Men frequently showcase excessive daytime sleepiness, while women’s symptoms often lean towards fatigue, insomnia, or mood shifts.
Unique female conditions, such as hormonal changes and pregnancy, have potential implications on sleep patterns and may heighten sleep-disordered breathing. This can complicate the diagnosis process for women. The Epworth Sleepiness Scale, a trusted metric in sleep medicine, serves to assess levels of daytime sleepiness.
Considering these symptom variations, there’s a pressing call for gender-adapted approaches in the diagnosis and treatment of this sleep disorder. Adopting such strategies ensures that both men and women are diagnosed accurately and receive the appropriate care tailored to their specific needs.
Risk Factors for Men and Women
One’s body mass index (BMI) can be a significant predictor of sleep apnea. Obese patients, irrespective of gender, demonstrate a higher susceptibility to the disorder. However, fat distribution varies between men and women.
Men often accumulate fat around the neck, which can increase upper airway resistance and the risk of airway obstruction. In contrast, women, especially post-menopausal, might see increased fat deposits around the upper airway, elevating their risk.
Anatomical and Biological Differences
Below are some of the key distinctions that shed light on how men and women uniquely experience sleep apnea, highlighting the male and female sleep apnea differences.
Upper Airway Structure
The design of the upper airway in men and women shows noticeable differences. Men generally have a broader airway diameter, which, while allowing for more airflow, can be more prone to collapsing, thus leading to obstructive sleep apnea.
On the other hand, women’s narrower airways might provide a certain degree of protection against the most severe instances of airway collapse. However, they can still be susceptible to sleep apnea under certain conditions.
Role of Hormones
Hormones, particularly progesterone, can influence sleep apnea risks. Progesterone is known to enhance the tone of the upper airway muscles.
In women, this hormone, at certain levels, offers protection against the condition by ensuring the upper airway remains open. However, events such as menopause, which result in decreased levels of female hormones like progesterone, can lead to an increased risk of sleep apnea in women.
Fat Distribution
Where the body stores fat plays a role in sleep apnea risks. Men often store fat around the neck, which can amplify the chances of the upper airway collapsing during sleep.
Women, especially during post-menopausal phases, might have increased fat deposits around the upper airway, which can alter its function and lead to sleep disturbances.
Tongue and Palate Architecture
The structures within the oral cavity, notably the tongue and soft palate, play a role in the pathogenesis of sleep apnea.
Men tend to have a larger tongue and a longer soft palate compared to women, which might increase the chances of airway obstruction during sleep. The spatial relationship between these structures and the available airway space can influence snoring and episodes of apneas, especially in men.
Neural Control and Responses
Neurological feedback mechanisms that control breathing during sleep might differ between genders. Men, for instance, might have a diminished arousal threshold, meaning they are less likely to wake up in response to breathing interruptions compared to women.
This differential neural response can contribute to more prolonged and frequent apneic events in men than in women, even if both genders experience the same degree of airway obstruction.
Diagnostic Procedures
Professionals need a thorough understanding of the patient’s symptoms and sleep patterns to diagnose sleep apnea, considering the sleep apnea variations by gender. Both genders, when showing signs of obstructive sleep, must undergo specific tests to determine the extent and nature of the disorder.
Polysomnography
This is the most common diagnostic sleep test. It’s a comprehensive recording of the bio-physiological changes that occur during sleep. Polysomnography monitors various body functions during sleep, including brain electrical activity, eye movement, muscle activity, heart rate, respiratory effort, airflow, and blood oxygen levels.
Home Sleep Tests
For some patients, home sleep tests might be recommended. These are simplified versions of polysomnography and can be done at home. They usually measure heart rate, airflow, breathing patterns, and blood oxygen levels. The choice between a polysomnography and a home sleep test often depends on the patient’s specific symptoms, underlying health conditions, and preferences.
Gender-Specific Considerations
During the diagnostic phase, it’s essential to consider gender-specific symptoms and risk factors. For example, women might present less frequently with loud snoring, a common symptom in men, and more often with fatigue or insomnia. These nuances can influence the direction and interpretation of sleep tests.
Treatment Modalities and Their Efficacy in Both Genders
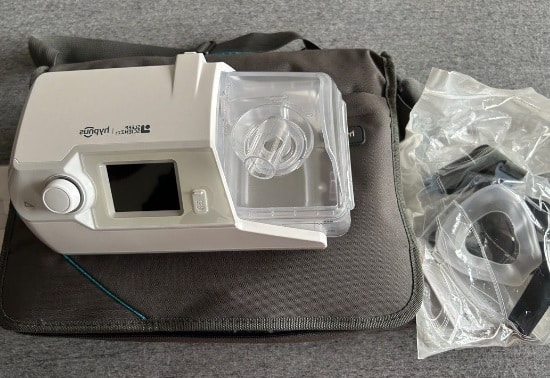
CPAP stands out as the primary treatment for OSA. It works by delivering a steady stream of air through a mask to keep the upper airway open. While both men and women benefit from this treatment, there are some differences worth noting:
- Compliance: Some studies indicate that women might consistently use their CPAP devices regularly. This could be due to different discomfort experiences or symptom relief immediacy.
- Mask Fittings: Women and men have different facial structures, which can influence mask fit. Manufacturers are now designing masks specifically for women to address these unique needs.
Lifestyle Modifications
Apart from medical interventions, lifestyle changes can play a pivotal role in managing sleep apnea.
- Weight Management: Maintaining a healthy weight can reduce sleep apnea symptoms. Given the differences in body fat distribution between genders, men might see improvements by reducing neck fat, whereas women might benefit from overall weight loss.
- Positional Therapy: Some people experience sleep apnea primarily when sleeping on their back. For them, sleeping on their side can help. While this strategy benefits both genders, men, due to their anatomy, might find it more effective.
Also Read: Enhancing Sleep Quality: CPAP Tips & Lifestyle Changes
Oral Appliances
Another treatment option is dental devices or oral appliances. These devices are designed to keep the throat open by either holding the tongue or supporting the jaw in a forward position. They’re especially useful for people who can’t tolerate continuous positive airway pressure (CPAP). Both men and women can use these, but it’s essential to get a proper fit.
Surgical Options
In cases where other treatments don’t provide relief, surgery might be recommended. Procedures can range from removing excess tissue from the throat to more complex surgeries like jaw repositioning. The efficacy and suitability of these procedures can vary, but gender-specific anatomical differences might influence the decision-making process.
Final Thoughts
Sleep apnea is more than just an interruption in breathing during sleep; it’s a condition influenced by various factors, including one’s gender. Understanding how is sleep apnea different in men and women is crucial.
Gender differences play a significant role in how the disorder presents, its prevalence, and the efficacy of treatments. Men might be diagnosed more often, but emerging insights suggest women’s symptoms can be overlooked or misinterpreted. As these differences become clearer, medical professionals must adapt, ensuring everyone gets the precise care they need.
For those looking to enhance their sleep apnea management, quality accessories can make a significant difference. Thanks for reading! Explore and shop Resway’s top-rated CPAP accessories on Amazon.
Did this article help you? Let us know in the comment section below!




